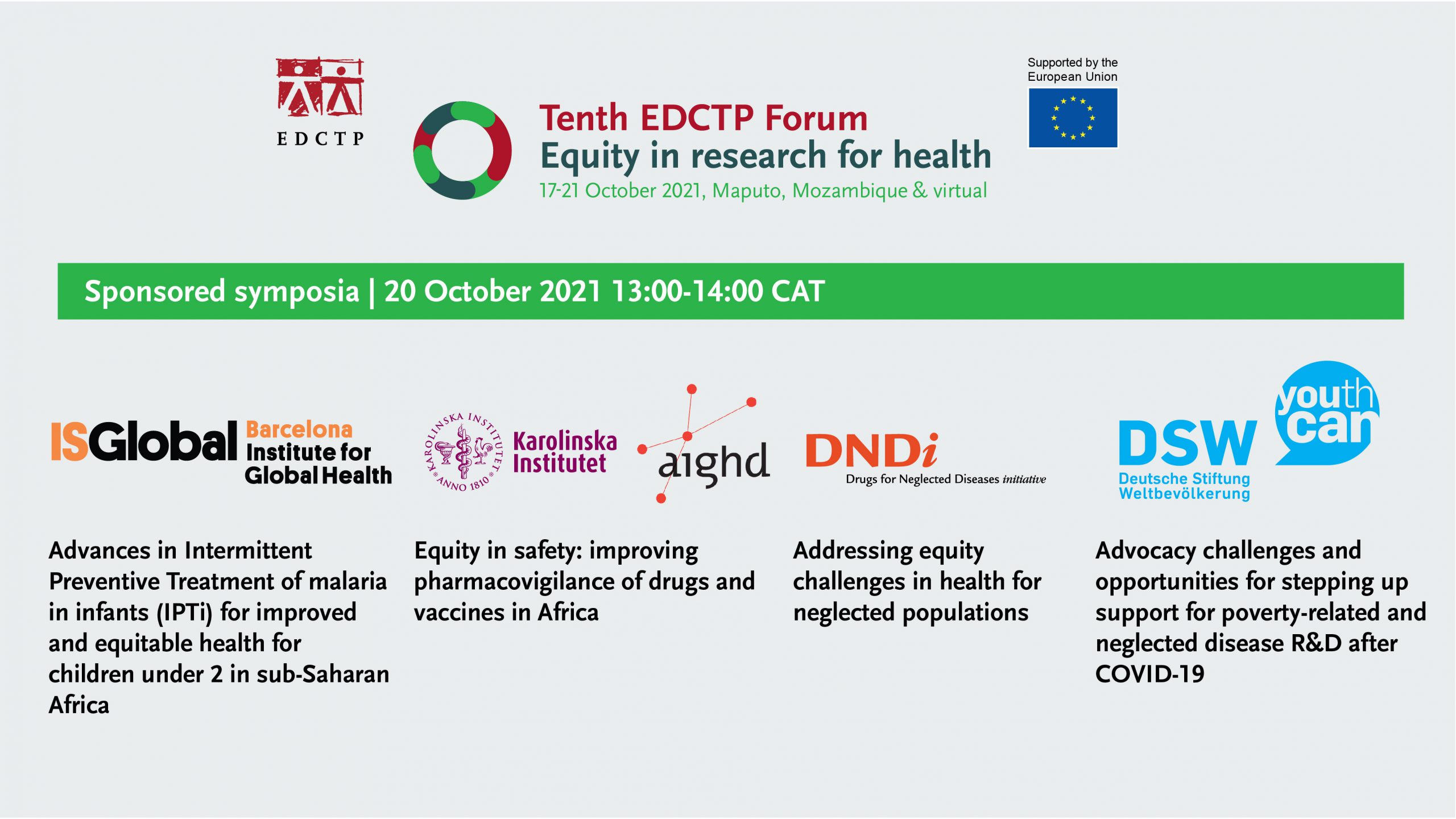
On Wednesday 20 October, sponsored symposia were organised by Barcelona Institute for Global Health (ISGlobal), Amsterdam Institute for Global Health and Development (PAVIA project) & Karolinska Institutet (PROFORMA project), Drugs for Neglected Diseases initiative (DNDi) and Deutsche Stiftung Weltbevoelkerung (DSW).
By Paul Chinnock
ISGlobal | Advancing biomedical interventions towards improved and equitable health (Malaria): Advances in Intermittent Preventive Treatment of malaria in infants (IPTi) for improved and equitable health for children under 2 in sub-Saharan Africa
This session was kindly sponsored by the Barcelona Institute for Global Health (ISGlobal) and chaired by Clara Menendez (ISGlobal).
Lessons learned after four years of IPTi implementation in Sierra Leone
Augustin Fombah (ISGlobal and Ministry of Health of Sierra Leone) gave the first presentation. Malaria remains a major problem in Sierra Leone; prevalence in children is only 6% in the Western Area Urban district but ranges from 26-58% elsewhere in the country. Dr Fombah also outlined the progress of the expanded programme of immunisation (EPI) in Sierra Leone.
Dr Fombah gave a brief history of malaria interventions in Sierra Leone, beginning with the Roll Back Malaria initiative in 2004. A five-year plan launched in 2010 aimed to reduce mortality and morbidity by 50% and 75% respectively by 2015; rapid diagnostic tests were also introduced. A plan for 2016 to 2020 included the introduction of intermittent preventive treatment for pregnant women (IPTp) and infants (IPTi), along with improving case management and vector control.
The rationale for IPTi and the policy adopted in Sierra Leone was then described by Dr Fombah. WHO recommends the administration of sulphadoxine-pyrimehamne (SP) at intervals corresponding to routine vaccination schedules during the first year of life. In Sierra Leone it is delivered through routine EPI clinic activities. IPTi was launched as a pilot programme in March 2017 in one district in each of the country’s four regions. Infants received IPTi at 10 weeks, 14 weeks and 9 months. The programme was reviewed and lessons learned. It was considered to be successful and rolled out in all 12 districts of the country in 2018.
IPTi coverage rate 2016 to 2020 has shown considerable growth. In 2020 over 80% of children received all three treatment doses. The case rate in children under one year has fallen during that same period, which may be partly explained by expansion of the IPTi programme though valid conclusions cannot yet be drawn on that point.
Successes have included the high level of community trust and acceptance that has been achieved, the successful introduction of IPTi into the EPI, and the establishment of technical working groups. Constraints have included inadequate resources, initial poor recording, irregular site-level supportive supervision, and delays in drug procurement leading to intermittent stock-outs.
Recommendations based on the lessons learned are: conduct robust community information campaigns, establish technical working groups, ensure that adequate resources are made available and strengthen drug procurement systems.
Challenges in the implementation of IPTi in a country with different malaria transmission patterns
Francisco Saúte, Manhiça Health Research Centre (CISM, Mozambique) began by describing malaria transmission and control in Mozambique, referring to Massinga District where his project is located. Transmission rates vary from 1% in the south of the country to nearly 60% in the north. Within regions, and even within districts, there are wide variations. Strategies for malaria control recommended by WHO have been introduced, including: long-lasting insecticidal nets (LLINs), IPTp, prompt diagnosis and treatment, behaviour change communication and targeted indoor residual spraying (IRS) in some areas. Success in rolling out the interventions has varied across regions. Areas most in need of effective malaria control are not always those where implementations have been most effectively introduced.
In Maputo Province, transmission is very low and a ‘differential approach’ is now being adopted; LLIN distribution has been discontinued and IRS has moved from a blanket to a focal approach. Other interventions will continue but it remains to be seen whether an IPTi programme is introduced here.
Dr Saúte then briefly listed ongoing operational research relevant to malaria control. In addition to IPTi, the impact of house improvement is being investigated in a current study. Mass administration of ivermectin is now being conducted for other parasitic conditions; it will be interesting to see whether this might have an impact on malaria transmission, given that the drug is toxic to mosquitoes.
Overview of the MULTIPLY project (MULTIple doses of IPTi): a Lifesaving high-yield intervention) project in Mozambique, Togo and Sierra Leone
Clara Menendez (ISGlobal) began by giving a background to the development of IPTi and other forms of malaria chemoprevention and she reviewed the many studies published since 2001, which have found high levels of efficacy.
IPTi has been recommended by WHO since 2010, in areas of moderate-to-high malaria transmission where resistance to sulphadoxine-pyrimethamine (SP) is not high. It is co-administered with routine vaccinations for measles and DTP (diphtheria-tetanus-pertussis). It is one of the most cost-effective strategies for malaria control, as it uses an inexpensive drug (SP) and is based within an existing health scheme (EPI). Guidance on its use is readily available from WHO. However, so far it has only been implemented in Sierra Leone.
Dr Menendez says ‘the momentum is now’ to implement IPTi more widely. The necessary synergies have already been created between many stakeholders, including funding agencies such as EDCTP.
She summarised the recently launched MULTIPLY project, which aims to administer multiple doses of IPTi and expand the intervention into the second year of life, with doses given at EPI contacts for vaccinations and vitamin A supplementation. With EDCTP funding, MULTIPLY will take place (May 2021 to August 2024) in Sierra Leone, Togo and Mozambique (sample size 45,000 children under two years). These are all areas of moderate-to-high and high seasonal transmission. Results from the different countries will be instructive to compare: all have EPI systems but with different levels of coverage, Sierra Leone is already implementing IPTi in children under one year but Togo and Mozambique do not have such a programme in place.
The primary objective of MULTIPY is to implement and increase the uptake of IPTi. Secondary objectives include assessment of the operational feasibility, cost-effectiveness and acceptability of the intervention, and also its impact on malaria prevalence and incidence rates. And it will be interesting to see whether the introduction of IPTi might increase demand for EPI vaccines.
An important question is whether IPTi (and IPTp) will still work in areas of high levels of SP resistance. (One study has already found that effectiveness of IPTp is compromised in such settings but is still associated with increases in maternal haemoglobin and in birth weight.)
Dr Menendez thanked all the many partners involved in this major project.
AIGHD & KI | Equity in safety: improving pharmacovigilance of drugs and vaccines in Africa
Within the track Equity challenges in cross-cutting issues (pharmacovigilance), the Amsterdam Institute for Global Health and Development (AIGHD) and Karolinska Institutet (Sweden) kindly sponsored a session on the PROFORMA and PAVIA projects, together with a presentation on COVID-19 vaccine safety surveillance in Africa. It was chaired by Sten Olsson (United Kingdom) and Margareth Ndomondo-Sigonda (South Africa).
Strengthening pharmacovigilance in mass drug administration and immunisation programmes: experience from the PROFORMA project
Eleni Aklillu Karolinska Institute (Sweden), explained that PROFORMA is a five-year, EDCTP-funded project to strengthen pharmacovigilance and post-marketing surveillance in Kenya, Ethiopia, Uganda and Tanzania. She shared some of the experience gained over the last three years.
Sub-Saharan Africa has seen increases in: access to drugs, clinical trials, vaccination and mass drug administration (MDA). However, there is limited coordination between national medical regulatory authorities (NMRAs) and public health programmes (PHPs) to monitor drug safety.
PROFORMA has adopted a trilateral partnership between academia, trainers and stakeholders (including WHO and PHPs). Training of trainers for sustainability and training to change policy into practice are key elements of the programme. This is a joint venture between the Karolinska Institute and four African universities, plus NMRAs in each of the four African countries and WHO collaborating centres in pharmacovigilance.
The general objective is to strengthen national pharmacovigilance infrastructure and the post-marketing surveillance system in the four African countries, identifying gaps, needs and priorities. Training is comprehensive, addressing nine different categories. MDA safety monitoring and vaccine surveillance are important elements of PROFORMA.
Launch meetings were carried out in 2018 in each country. A comparative study of the four countries has already been published, with the main finding that there was little or no collaboration between NMRAs and PHPs for adequate to enable effective safety monitoring.
Activities included: ethics application and approval, stakeholder meetings, the development of workplans, training for data collectors, the development of a database, and field work. (School teachers, as well as health personnel were used as data collectors.) Human papillomavirus (HPV) vaccine surveillance workshops were held in Tanzania and Ethiopia. In one study, efficacy and safety in patients receiving praziquantel MDA was monitored.
A range of activities in all the countries was described, much of this being field work (sometimes in difficult circumstances). The PROFORMA team have also been involved in curriculum development and e-learning. Five PhD students are being trained at the Karolinska Institute. Studies from Kenya (MDA safety and tolerability), Tanzania, Rwanda (effectiveness of MDA after 10 years) and Ethiopia have now been published and other data are now being analysed.
Expected outcomes include more people with pharmacovigilance training (7 PhD, and 5 MSc), improved infrastructure and regulatory capacity, improved undergraduate and postgraduate training in pharmacovigilance for sustainable collaboration between NMRA, PHP and academia.
Making safety surveillance work: Lessons learnt from the PAVIA project
Yohanna Avong, Institute of Human Virology (Nigeria), explained that PAVIA means Pharmacovigilance in Africa and went on to describe the background to the project. In particular, PAVIA is looking at new medications for treating multi-drug-resistant TB (MDR-TB). The introduction of new drugs in Africa is often based on limited trial data. Pharmacovigilance in Africa, therefore, needs urgent strengthening. PAVIA aims to achieve this through governance and financial sustainability, optimising surveillance systems, human capacity development, supporting the use of technology, and monitoring adverse drug reaction (ADR) reporting. The new MDR-TB drugs are being used as a pilot.
PAVIA has two major stakeholders – Africa and Europe. The African countries involved are Nigeria, Eswatini, Ethiopia and Tanzania. In Europe it is the Netherlands and Italy. Specific roles have been given to institutions within those countries. These institutions include research centres and national regulatory authorities. International stakeholders include WHO, the African Union and other African regional bodies, the International Society of Pharmacovigilance and the Bill & Melinda Gates Foundation. We therefore speak of PAVIA as a Consortium.
The ‘PAVIA triangle’ approach adopted involves medical research institutes, treatment sites/hospitals and public health programmes. In each country these organisations will work together. Baseline assessments have been conducted in the four African countries and gaps have been identified in: policy, law and regulation; systems structure and coordination; signal generation and data management, training, support for electronic tools. Countries were found to be at different levels in many cases.
Specific roadmaps have now been developed for each country in terms of: mission, vision, objectives, strategy and action plan. A blended learning package has been developed involving both face-to-face and e-learning. A cascade approach for training has been introduced. Dr Avong gave some examples of how this is being done in Nigeria. A key requirement is to optimise ADR reporting among partner countries. PAVIA is also promoting e-tools for prompt and accurate ADR reporting, including the use of a new app.
Sustainability is built on: hosting of resources at partners’ sites, the triangle approach, and training of trainers. Dr Avong believes that PAVIA is already changing the pharmacovigilance landscape in Africa.
COVID-19 vaccine safety surveillance in Africa
Sujeet Kumar Jain, WHO-AFRO (Republic of Congo) explained that an adverse event following immunisation (AEFI) is any untoward medical occurrence which follows immunisation. (It does not necessarily have a causal relationship with vaccine usage.) There can be five causes of an AEFI: vaccine-product-related reaction, vaccine quality defect-related reaction, immunisation error-related reaction, immunisation anxiety-related reaction, or a coincidental event. Dr Jain went on to say more about how vaccine reactions can be classified, considering each of the five causes in more detail. (In the COVID-19 context it may be difficult to recognise the cause as the vaccines are so new there is very little data and we don’t yet know about long-term side effects.)
The key players and their roles within the AEFI monitoring cycle next received Dr Jain’s attention. They are: programme managers, caregivers, health workers, national vaccination teams and the AEFI committee. Different countries follow different protocols. He gave the example of Mozambique. Regular support is provided to countries by PAVIA to ensure a functional surveillance system, by meeting minimal capacity for vaccine safety.
Dr Jain very briefly set out the key vaccine safety strengthening activities that have been recently issued by WHO in the COVID-19 safety context. 40 African countries have now reported 22,041 cases of AEFI following COVID-19 vaccination, including 1,803 serious cases. (There has been a huge variation between countries.) Areas for further improvement have been identified by PAVIA: regular line listing of cases, timely investigation, documenting AEFIs using multiple COVID-19 vaccines simultaneously, and the handling of communication challenges including media and community safety concerns.
DNDi | Addressing inequities in research (Equity challenges): Addressing equity challenges in health for neglected populations
This symposium was sponsored by the Drugs for Neglected Diseases initiative (DNDi). The Chair was Fabiana Alves (DNDi, Switzerland)
Progress and challenges in meeting the NTD Roadmap goals
Anthony Solomon of the World Health Organization’s (WHO) Department of Control of Neglected Tropical Diseases (NTDs) gave the first presentation. Infectious diseases are now very much in our minds but while the world focuses on COVID-19, NTDs continue to wreak havoc on millions of lives. Some NTDs are now causing more problems than before the start of the pandemic. If we are going to build a better world after the pandemic, then part of this must be to step up action against NTDs, the root cause of which is poverty. NTDs themselves cause poverty and economic losses.
He went on the remind us of the diverse range of organisms responsible for the main 20 or so NTDs. Why have we not defeated them yet? It is because we have not tackled poverty.
Dr Solomon said his intention was not to just talk about problems but also solutions. There are simple cost-effective ways to break the cycle of inequity response for the continuing prevalence of NTDs. These include: early diagnosis and treatment, quality care, preventive chemotherapy and vector control, and cross-cutting approaches (for example collaboration with water and sanitation programmes).
Progress has been made; 43 counties have eliminated at least one NTD. Dr Solomon gave instances of successes achieved (e.g. human African trypanosomiasis has been reduced by 97% since 2010). Over a billion people worldwide are now receiving NTD treatments every year, usually delivered by community workers. However, progress has not been uniformly good. For example: the 2020 target for trachoma elimination (set in 1996) has not been achieved, there have been problems in treating onchocerciasis in hypo-endemic areas, and the eradication of Guinea worm disease has been delayed. Factors that explain these failings include: poor quality data, lack of epidemiological understanding, lack of diagnostics and treatment, and insufficient funding and support.
The Roadmap for NTDs (2021-2030) has been produced after careful review of the successes and failures. It is written by and for the global community of people who work in NTD programmes. It calls for three fundamental shifts: a move from measuring process to measuring impact, a move from vertical/top-down planning to holistic/cross-cutting approaches, and a shift towards country ownership and domestic funding. Endemic countries must take the lead in decision making. Overarching and cross-cutting targets are laid out in the Roadmap, in addition to more specific targets for individual diseases.
We must now work to integrate NTD activities into broader health programmes. Dr Solomon said ‘NTDs relate to sustainable goals in a way that is mutually reinforcing. In taking NTD control to remote populations, we should also seek to improve their access to comprehensive primary health care’.
COVID-19 has caused disruption to NTD programmes, including preventive chemotherapy campaigns, education and awareness activities, and support for self-care and rehabilitation. If we are going to ‘build back better’ we must include action against NTDs in our efforts.
Human African trypanosomiasis: New treatments for the population at risk
The audience watched a short video about Human African trypanosomiasis (HAT) describing the use of the drug fexinidazole (developed by DNDi and manufactured by Sanofi) in the Democratic Republic of Congo [1]. Antoine Tarral (DNDi, Switzerland) then gave his presentation. The development of a one-dose cure to sustain elimination (with few adverse effects) has been a revolution. Treatment formerly involved an arsenic-based compound with many side-effects (melarsoprol), feared by patients and doctors. Nifurtimox-eflornithine combination therapy (NECT, introduced by DNDi in 2009) is much superior but hospital-based, bulky and requiring complex logistics. Fexinidazole is patient-centred, easy to use and taken once a day for 10 days. Currently in development from DNDi is Acoziborole – hoped to be a cure requiring just one dose.
Dr Tarral presented some recent data on HAT prevalence. It is hoped to achieve further progress towards elimination. This will require measures that include rapid diagnostic tests and remote testing, access to effective treatments, and community involvement in tsetse fly control. Treatment must also be extended to individuals at risk.
WHO HAT goals for 2030 include the interruption of transmission of gambiense HAT, in response to which DNDi is developing Acoziborole for extended use in the population, including children. WHO also seeks to keep rohodesiense HAT eliminated as a public health problem. DNDi is working towards the registration of Fexinidazole to help achieve this.
Improving cryptococcal meningitis treatment therapies for people living with HIV
A video on cryptococcal meningitis (CM) explained that it is the second leading cause of death in people with HIV (after TB). It is responsible for 180,000 deaths per year. Managing the condition is very labour intensive for the health workers involved. A better treatment is needed, which also needs to be more affordable and accessible.
Isabela Ribeiro, (DNDi, Switzerland) began by stressing that HIV thrives on inequity and inequality. Mortality is still high and poor health services are common in areas (such as Africa) where HIV rates are high. Antiretroviral (ARV) scale up is obviously the ultimate key to reducing CM mortality in people with HIV. This has been established in Europe and North America. Retention of patients on ARV is crucial; many African CM patients are people who began ARV treatment but were unable to continue with it.
Dr Ribeiro described CM as a neglected disease; it receives very little research funding, yet it accounts for 15-20% of HIV-related and other deaths in both Africa and Southeast Asia. Even with treatment, mortality is 20-70%. It is an indicator of health system failure and existing inequalities.
The main treatment drug in developing countries is currently fluconazole which achieves only a 20% survival rate. Diagnostics also needs to be improved. DNDi is working in flucytosine, an old anti-fungal drug, to create a sustained release medication that would greatly simplify inpatient and outpatient treatment. Dr Ribeiro described the key steps in the plan for its clinical development and ultimately. A number of partners are involved, including EDCTP. Advocacy efforts will also be undertaken.
New treatments to respond to the needs of neglected patients affected with leishmaniasis
A video reminded the audience of the disease burden that visceral leishmaniasis (VL), also known as Kala azar, still exacts in many parts of Africa, South America and elsewhere. It persists on poor, remote and politically unstable areas, with 200,000-400,000 new cases reported annually. East Africa is the worst afflicted area. The video referred to the work of DNDi’s Leishmaniasis East Africa Platform (LEAP). See also: https://dndi.org/global-networks/leap-platform/
Fabiana Alves, DNDi (Switzerland) gave further background on VL, referring also to cutaneous leishmaniasis (CL). There are five current VL treatment drugs but they all have limitations, including serious toxicity issues. She very briefly outlined the DNDi VL programme strategy. This includes efforts to use existing drugs in new formulations and combinations but DNDi has also invested in a search for new compounds.
Combination therapies investigated have included paromomycin-miltefosine combination therapy, with which trials are continuing in Africa and Asia. Problems have been encountered and regimens adapted. It is now looking like this will offer a better treatment, well suited to children.
HIV-VL patients are the most difficult to treat and require special case management. In Ethiopia, 20% of VL patients are also HIV-infected. DNDi is investigating the use of AmBisome monotherapy and AmBisome-miltefosine combination therapy.
Dr Alves emphasised that these are just examples of the possible new treatments being pursued but the big difference will come with discovery of new compounds. These must be: oral, well-tolerated, have improved efficacy, be suitable for use at primary health care level, and be affordable. Such a new treatment would also help break the cycle of infection, and it would additionally benefit CL patients.
1 EDCTP has funded the FEX-g-HAT project which is facilitating access to (delivery and uptake of) fexinidazole in Africa
DSW | Advocacy challenges and opportunities for stepping up support for poverty-related and neglected disease (PRND) research and development (R&D) after COVID-19
Deutsche Stiftung Weltbevoelkerung (DSW) organised this session within the track ‘Capacity strengthening, collaborations, enhancing the research environment, knowledge translation (Partnership and alliances to enhance coordination, collaboration and cooperation)’.
Agustín Martín Lasanta, Senior Advocacy officer at DSW Brussels, both chaired the symposium and gave a short opening presentation. He explained that the purpose of the symposium was to look at the impact of COVID-19 on research on poverty-related and neglected disease, both in terms of scientific developments and as regards changes to the global policy and funding landscape. The risks and opportunities resulting from the pandemic would also be examined.
EU-Africa successes have included the development of combination therapies and repurposed vaccination platforms, repurposed diagnostics, and R&D in epidemic preparedness. New technologies used against COVID-19 could now be used against neglected diseases, for example mRNA vaccine technology. COVID-19 is not a neglected disease but should it be included within the remits of organisations like EDCTP? Many EU-Africa tools have been developed that can assist in epidemic preparedness and health security.
Dr Lasanta hoped the discussion today would help members of the audience in their advocacy work and in attracting new funding.
A more enabling environment for PRND R&D in Africa: challenges & opportunities
Bartholomew Dicky Akanmori, Regional Advisor for Vaccination Research, WHO-AFRO (Republic of Congo) began by reminding the audience of the negative consequences of inequity in research for interventions on poverty-related and neglected diseases (PRNDs). Inequity leads to delays in the development of new interventions and hinders countries in their progress towards achieving the Sustainable Development Goals. One of the lessons learned from COVID-19 is that progress can be achieved through global solidarity, innovation priority setting, capacity building, accelerating R&D and access to vaccines. It has also been made clear that African leadership can play a key role in the development and registration of new products.
Nevertheless, challenges remain for research and development against PRNDs. New and better diagnostics, treatment and vaccines are still needed, in addition to improvements in other preventive strategies. He paid tribute to the work of EDCTP, stressing the need for it to include technology transfer and regulatory systems strengthening in its programme. This would assist in the move towards smart, innovative and focused public health. Collaboration with industry would also help establish more manufacturing sites in Africa.
If PRNDs are not addressed by African countries themselves, we will continue to have the inequities which exist right now in the research and development of products for these diseases.
Funding for neglected disease R&D: risks, opportunities and expectations
Nick Chapman, Chief Executive Officer of Policy Cures Research (Australia), focused on the risks to funding for PRND research and development that may result from the COVID-19 pandemic. It is not yet clear what kind of impact there may be, but it is the kind of issue that Policy Cures’ G-FINDER project is well placed to investigate.
G-FINDER retrospectively collects data on the funding landscape but does not yet have all the data on 2020 that it will need to compile a report. Before COVID-19, the PRND research landscape was probably the best it has ever been; funding had risen steadily for the previous five years across all sectors and diseases. While funding levels were still not at the level that they really need to be (particularly with regard to the neglected tropical diseases), we had a ‘fairly positive picture’. Referring to the 2014-2015 West African Ebola epidemic, Dr Chapman said that, at that time, some funding was diverted towards Ebola programmes but the negative effect of this on PRND funding was only short-term. In the longer term, the Ebola epidemic may even have led to increases in PRND funding.
Will the damage that COVID-19 is doing to economies lead to a reduction in PRND funding? G-FINDER historical analysis has found that changes in GDP seem to have little impact on funding, though falls in GDP do generally have a negative effect on government overall expenditure, particularly on overseas development assistance. (Interestingly some of the biggest rises in research funding came after the global financial crisis of 2008-2009.)
Dr Chapman believes that given the nature of the pandemic it is likely that there will be a protective effect on PRND research funding. Although we are yet to see the effects of the pandemic on PRND research funding, there is good reason to be optimistic.
Highlighting the value of PRND R&D during the COVID-19 pandemic
Marleen Temmerman, Chair of the Department of Gynaecology & Obstetrics, Aga Khan University (Kenya), began by quoting from a recent paper (Blinken and Becerra, JAMA 2020) arguing that regional public health organisations should be more involved in priority setting as well as implementation. The international community, regional bodies, in addition to countries themselves, should ensure the availability of adequate funding.
Prof. Temmerman went on to describe the work of the Advisory Group on Research and Innovation (R&I) for Africa-Europe Cooperation, in which a working group (September 2021) focused on the need to improve health systems, strengthen R&I capacities, support the ‘innovation and technology revolution’ and promote a ‘green transition’ in Africa. Issues identified included: that more investment is needed against poverty-related and neglected diseases; that EDCTP has successfully developed collaborations across Africa and the EU against these diseases; Africa-EU cooperation needs to be reinforced, particularly with regard to supporting late-stage clinical research of upcoming clinical products; and that Africa and the EU should encourage more ‘EDCTP-like’ collaborations in other areas of health cooperation – such initiatives play an important role in strengthening epidemic preparedness and health security.
The meeting recommended for increased AU-EU collaboration: research and innovation to strengthen health systems; improving the ethics and regulatory environment; and, crucially, moving from R&I to policies and practices that make a difference. Better alignment is needed between EU programmes in Africa, in particular with regard to research and development. African nations must be more involved in the design and development of EU-supported initiatives in Africa. The role of embassy delegations is extremely important in ensuring that the policies adopted are relevant to local needs. The current R&I dialogue between Africa and the EU should be more inclusive, with full involvement of all stakeholders. It is important that these recommendations are considered within the international summits now taking place to address the emergency created by COVID-19.
The EDCTP3 Strategic Research Agenda: harnessing COVID-19’s momentum to advance PRND R&D
Catherine Hankins, Deputy Director of Science at the Amsterdam Institute for Global Health and Development (The Netherlands), began with a review of EDCTP2’s activities, which have taken place in 19 European and 41 African countries. To date, €814m has been awarded; over 140 collaborative research grants have been awarded, there have been 90 grants to strengthen clinical research capacity, and 200 fellowship grants have been awarded to support the career development of African scientists.
The impacts of COVID-19 on EDCTP-funded projects have included: delays and disruptions, extended timelines for ethical and regulatory approvals, restrictions affecting transport of essential equipment, expiry and shortage of medicines and trial investigational products, the closure of institutions, and bans on meetings. The delays have had a knock-on effect on other projects.
Meanwhile the pressure and workloads on clinicians and researchers in both Africa and Europe have increased. The closure of schools and childcare facilities has increased those pressures, particularly on women. Project costs have risen and there have been impacts on fellowships and on students. Professor Hankins highlighted the position of the Democratic Republic of Congo, where the focus on COVID-19 and Ebola has led to suboptimal vaccination efforts and the potential threat of resurgence of other vaccine-preventable diseases. However, the capacity and experience built during the Ebola virus outbreak were used in the response to COVID-19.
Since the start of the epidemic, EDCTP has been collaborating with several major initiatives. In its strategy and prioritisation, EDCTP has had to consider a number of questions: does COVID-19 disproportionately affect people in sub-Saharan Africa; is there a need for new or improved medical products; is there a commercial market to attract private industry; are there potential medical products worth considering for progression in clinical development; are other funders better placed and already investing sufficiently in these priority areas, and is there sufficient justification for EDCTP to prioritise this disease?
Moving on to the development of the Global Health EDCTP3 Joint Undertaking, she said that key features of the new programme would include a greater emphasis on phase III and IV trials and product-focused implementation research, and a recognition of the changes in clinical trial regulations that will revolutionise the way trials are run. GH EDCTP3 will also recognise the importance of emerging and re-emerging diseases, climate-crisis-related infectious disease, antimicrobial resistance, and co-infections and morbidities. An integrated approach will be adopted that focuses on clinical research, but which has capacity building as a built-in feature.